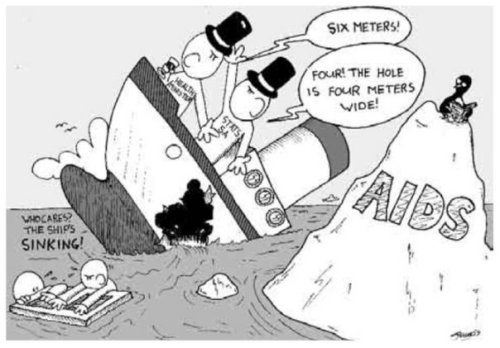
Since the foundation of the NHS, people have been fretting that its universality might lead to it being ‘abused’ by visitors from other countries.
In his 1952 book In Place of Fear, Nye Bevan argued that such comments were ‘ill-informed and some…deliberately mischievous’. Bevan noted that a charging programme would require ‘British citizens to carry means of identification everywhere to prove that they are not visitors’. He concluded that, given the limited burden overseas visitors were then placing upon the NHS, ‘What began as an attempt to keep the Health Service for ourselves would end by being a nuisance to everybody. Happily, this is one of those occasions when generosity and convenience march together.’
Recent years have seen intense pressure from certain sections of the media to restrict the access that migrants have to NHS services. In the 2004, the then Labour Government responded by introducing a charging regime for certain groups of ‘overseas visitor’ seeking to access NHS secondary care. They acknowledged (see response to Q210) that they did this in the absence of any evidence of the extent of the ‘abuse’ that the regulations were intended to address. Unsurprisingly, in the years since the regulations were introduced, they have led to vulnerable individuals coming to harm. The following accounts come from a set of case studies published by the Refugee Council…
‘E, a young woman from China, was turned away several times by her local NHS trust, who told her that unless she could pay them several thousand pounds upfront, they would not support her through the birth of her baby. She gave birth at home, with no medical care, and then both she and her baby had to be admitted to hospital with serious health problems relating to the traumatic birth. Once discharged, the hospital continued to send E bills, which frightened her so much she fled her home. The whereabouts of her and her child are not known.’
‘G, is an Arab man whose nationality is disputed. He suffers from bowel cancer, and was admitted in an emergency because of uncontrolled bleeding. The clinicians in A&E scheduled him for an operation as soon as the bleeding stopped. However, once the hospital discovered G was a refused asylum seeker, he was given a bill for many thousands of pounds, and his operation was cancelled. He was discharged from hospital and told to come back “when his condition deteriorates”.’
A new Department of Health consultation seeks to restrict migrants’ access to NHS primary care, a proposal that will certainly increase the risk that vulnerable individuals will come to harm. The only serious research on overseas visitors use of NHS primary care, conducted by Imperial College London, concluded that, given the ‘the limited financial burden that Overseas Visitors appear to be having on primary medical services’, the bureaucracy required to operate a charging regimen would be hard to defend even on cost effectiveness grounds.
I would encourage healthcare workers to submit responses to the consultation – humane and rational voices need to be heard in this debate. The deadline for responses is 28 August.
I have copied sections of my response below, which you could adapt if you make a submission. You may find this website, produced by a coalition of concerned NGOs, helpful too.
Question 1: Are there any other principles you think we should take into consideration?
Yes, several. The main additional principle that should be considered is this – policies that are likely to result in individuals coming to harm should only be considered if there is clear evidence that they are needed and if there are no alternatives.
There are a growing number of case studies describing individuals whose health has been placed at risk or who have come to harm as a result of the existing NHS charging regulations [1]. Extending charging into primary care can only exacerbate these problems.
For refused asylum seekers and undocumented migrants from outside the EEA, both the threat of charging and perceived links between the NHS and immigration services [2] are likely to deter patients from seeking help when they are unwell.
In your first principle, you have failed to understand that patients present with symptoms not diagnoses. Very often life threatening conditions present insidiously. Without access to routine investigations in both primary and secondary care, these conditions will be diagnosed late, leading to unnecessary suffering, onward spread of communicable disease and preventable mortality.
Making diagnostic services freely available might partially address this problem. However, this places healthcare professionals in the difficult position of being unable to treat patients with whom they have formed a therapeutic relationship (and to whom they therefore have a duty of care). It is also unreasonable to subject people to invasive diagnostics, x-ray irradiation, etc, if they may not be able to access treatment once a diagnosis is achieved.
That this is being discussed in the absence of evidence that ‘overseas visitors’ present a significant burden to the NHS speaks to the fact that ideology and cheap populism not evidence are driving this policy agenda. I am yet to meet a ‘health tourist’ in an NHS hospital.
The principle change proposed by this consultation is extending NHS charging into primary care. The only good evidence concerning use of primary care by ‘overseas visitors’ is the 2006 impact assessment conducted in Newham by academics from Imperial College London [3]. That survey found that charging for NHS primary care was unlikely be cost effective with the costs of operating a charging regime likely to be greater than any monies recovered from overseas visitors.
Question 2: Do you have any evidence of how our proposals may impact disproportionately on any of the protected characteristic groups?
It seems highly likely that individuals from ethnic minorities will be disproportionately affected by the proposed changes. Under the existing charging regime, we have not only seen those not entitled to care coming to harm [1]. We have also seen individuals from ethnic minorities who are entitled to free NHS treatment but have a poor understanding of or ability to express their rights coming to harm [1].
In the UK, there are already appalling racial inequalities in health outcomes. For example, Black African women are nearly four times more likely than White women to suffer a maternal death [4]. A significant number of these deaths are in women newly arrived in the UK who accessed antenatal care late. Given most women access antenatal care via their GP, restricting access to NHS primary care will exacerbate this problem.
Question 3: Do you have any views on how to improve the ordinary residence qualification?
I believe that if individuals are in the UK, they should be able to access healthcare and other essential services and to contribute towards these services by working and paying tax. If they are not lawfully in the UK, that is a matter for the immigration services. We should not be using denial of essential services – destitution and avoidable sickness – as a means to force individuals from the country. Such policies are inhumane and also unlikely to succeed, given most migrants are young and healthy with little need for healthcare or state support.
Question 5: Do you agree with the principle of exempting those with a long term relationship with the UK (evidenced by National Insurance contributions)? How long should this have been for? Are there any relevant circumstances under which this simple rule will lead to the unfair exclusion of any groups?
Entitlement to NHS services has never been based on tax contributions. Women who do not work outside the home, the disabled, children and others who have never paid National Insurance contributions can and should be able to freely access NHS care. The NHS should remain free at the point of delivery to all individuals in the UK. The policing of our borders is the responsibility of immigration officials not healthcare workers.
Question 6: Do you support the principle that all temporary non-EEA migrants, and any dependants who accompany them, should make a direct contribution to the costs of their healthcare?
No. If in the UK, they should contribute in taxation (VAT, income tax, etc) as others do and should be entitled to healthcare and other essential services. It is my understanding that such groups – largely young, healthy and in work – are already net contributors to the public purse.
Question 25: How can charges for primary care services best be applied to those who need to pay in the future? What are the challenges for implementing a system of charging in primary care and how can these be overcome?
Introducing charging for NHS primary healthcare would be a disaster. This is not the first time a Government has proposed such a change. When this was last proposed, dozens of healthcare workers took time to point out the many problems with the idea [5, 6]. These include…
– humanitarian concerns: the likelihood that vulnerable individuals will come to harm.
– cost effectiveness: primary care is cheap, prevents future need for expensive hospital care, and what evidence there is suggests that the costs of operating a charging regimen would be greater than any monies recovered [3].
– public health: loss of control over communicable diseases, with individuals with communicable disease unable to access diagnosis and treatment, and no opportunity to identify and vaccinate unvaccinated people residing in our communities.
It is not at all clear to me whether the issues raised in that consultation have been considered in these new proposals, which is unfortunate as healthcare workers are busy people and should not be required to make the same points again in multiple Government consultations.
Question 26: Do you agree with the proposal to establish a legal gateway for information sharing to administer the charging regime? What safeguards would be needed in such a gateway?
Unless the sharing of information is necessary to prevent serious harm, it is a basic tenet of medical ethics that data on health and usage of healthcare services will be treated as confidential. It would be totally inappropriate under any circumstances for any patient identifiable data to be shared with the immigration services and others not directly involved in clinical care. In Sweden, Medecins Sans Frontieres found that even the perception of links between the health and immigration services deterred vulnerable migrants from accessing healthcare [2].
1. First do no harm. London: Refugee Council, 2006. Available from http://www.refugeecouncil.org.uk/policy_research/research.
2. Experiences of Gömda in Sweden: Exclusion from health care for immigrants living without legal status. Stockholm: MSF Sweden, 2005. Available from http://www.rosengrenska.org/pdfs/ReportGomdaSwedenEn.pdf.
3. The identification and charging of Overseas Visitors at NHS services in Newham: a Consultation. London: Imperial College London, 2006. Available from http://www.lho.org.uk/viewResource.aspx?id=11948.
4. Saving Mothers’ Lives. London: CMACE, 2011. Available from http://www.rcog.org.uk/news/cmace-release-saving-mothers%E2%80%99-lives-report-%E2%80%93-reviewing-maternal-deaths-2006-2008.
5. Proposals to Exclude Overseas Visitors from Eligibility to Free NHS Primary Medical Services. A summary of submissions to a Department of Health consultation whose findings were never published. London: Global Health Advocacy Project, 2008. Available from https://www.researchgate.net/profile/Tom_Yates/contributions/?ev=prf_act.
6. Four Years Later: Charging Vulnerable Migrants for NHS Primary Medical Services. Students and junior doctors reveal the findings of an unpublished Department of Health consultation. London: Global Health Advocacy Project, 2009. Available from https://www.researchgate.net/profile/Tom_Yates/contributions/?ev=prf_act.